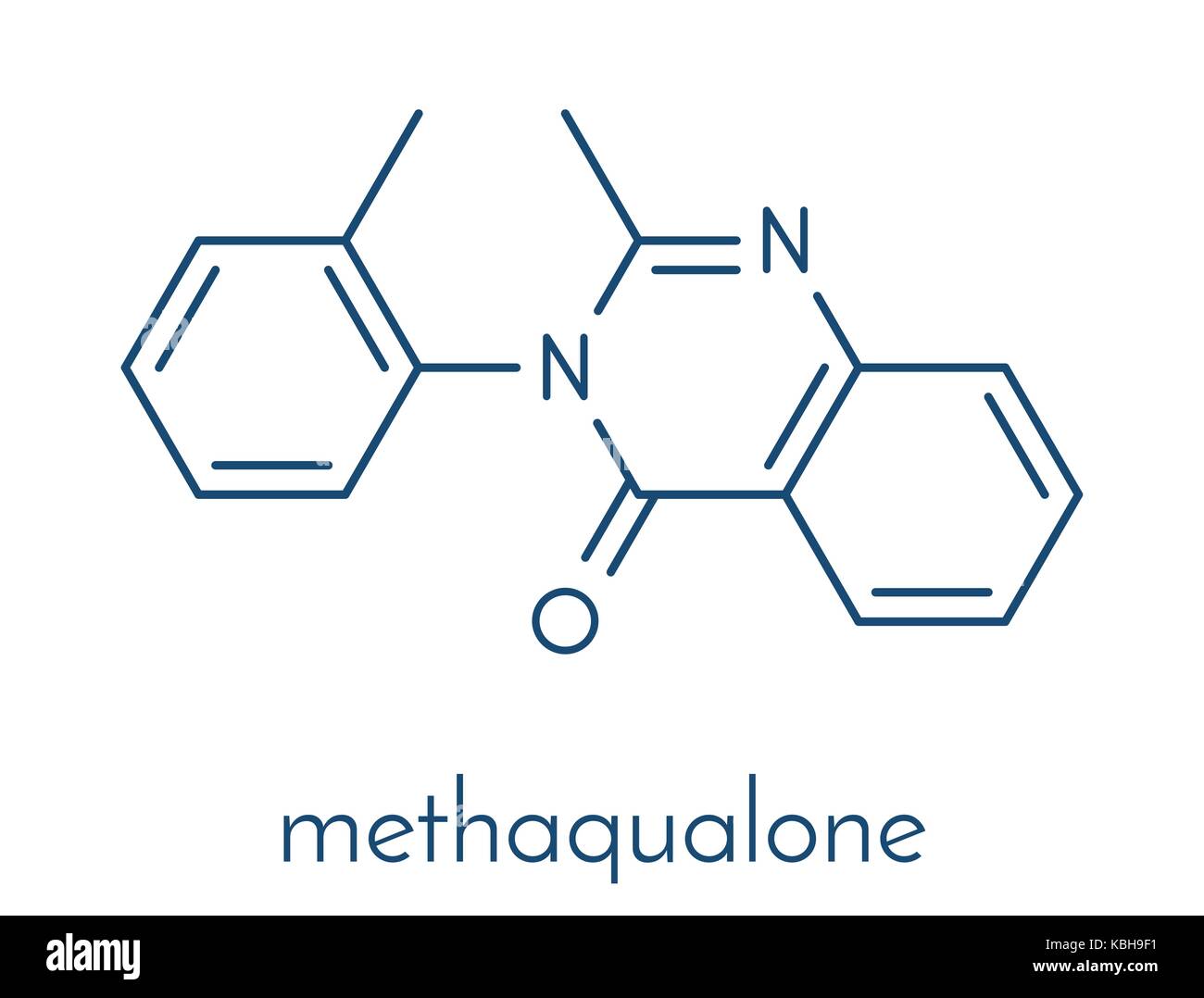
Methaqualone, a synthetic sedative and hypnotic drug, has long been a cause for concern due to its high potential for abuse and detrimental effects on health. Although banned in numerous countries, its illicit use continues to pose significant dangers to individuals and communities. Gaining a deeper understanding of methaqualone's impact is essential for raising awareness and combating its misuse.
Initially developed in India in 1951, methaqualone rose to prominence during the 1960s and 1970s as a prescribed treatment for sleep disorders and anxiety. However, its addictive properties and abuse potential soon became evident, prompting its prohibition in many parts of the globe. Despite its illegal status, the drug continues to circulate under street names such as "mandrax" or "quaaludes," posing ongoing risks.
This article delves into the multifaceted effects of methaqualone, exploring its implications for physical and mental health, societal challenges, and the necessity of addressing its misuse. By comprehending these aspects, individuals and communities can take decisive action to mitigate the drug's harmful effects.
Read also:Naughty America The Ultimate Guide To Exploring The World Of Adult Entertainment
Table of Contents:
- The Evolution of Methaqualone
- Physical Consequences of Methaqualone
- Mental Health Implications
- Addiction and Dependence
- Long-Term Impacts
- Broader Societal Effects
- Legal Framework and Regulation
- Treatment Approaches for Methaqualone Abuse
- Prevention Strategies
- Conclusion
The Evolution of Methaqualone
Methaqualone, once marketed as a safer alternative to barbiturates, gained rapid popularity due to its calming effects. However, its addictive nature soon surfaced, leading to its classification as a Schedule I controlled substance in the United States in 1984. This designation rendered it illegal to produce, distribute, or possess.
Origins and Development
Methaqualone was first synthesized in 1951 by scientists in India. It entered the market as a sedative-hypnotic drug under brand names such as Quaalude and Mandrax. Its popularity surged during the 1970s, particularly in the United States and South Africa, where it became a widely used recreational drug.
Decline and Prohibition
As addiction rates and overdose incidents mounted, governments around the world began to impose strict restrictions on methaqualone's use. By the late 1980s, the drug had been outlawed in most countries. Despite these measures, illicit production and trafficking persist in certain regions, notably parts of Africa and Asia.
Physical Consequences of Methaqualone
Methaqualone acts on the central nervous system, inducing sedative and hypnotic effects. These effects can result in both immediate and long-term physical consequences, impacting the body in profound ways.
Short-Term Physical Effects
- Slowed breathing
- Decreased heart rate
- Muscle relaxation
- Dizziness
- Blurred vision
Potential Risks
Even at low doses, methaqualone can impair coordination and judgment, heightening the likelihood of accidents. Overdose poses severe risks, including respiratory depression, coma, and death.
Read also:Remy Lacroix The Rising Star In The World Of Music
Mental Health Implications
Although methaqualone is primarily recognized for its sedative qualities, it significantly affects mental health. The psychological impact varies based on dosage, frequency of use, and individual susceptibility.
Psychological Impact
- Euphoria and relaxation
- Impaired cognitive abilities
- Memory loss
- Confusion
Long-Term Mental Health Risks
Prolonged methaqualone use can lead to serious mental health disorders, including depression, anxiety, and psychosis. These effects may persist even after the individual discontinues drug use.
Addiction and Dependence
Methaqualone is highly addictive, affecting both physical and psychological well-being. Regular consumption fosters tolerance, compelling users to increase their dosage to achieve the desired effects. This cycle intensifies the risk of dependence and addiction.
Signs of Addiction
- Intense cravings for the drug
- Difficulty reducing or stopping use
- Ignoring responsibilities
- Social withdrawal
Withdrawal Symptoms
Attempting to quit methaqualone can trigger uncomfortable withdrawal symptoms, such as anxiety, insomnia, and tremors. Medical supervision is often necessary to manage these symptoms effectively and ensure safety during the detoxification process.
Long-Term Impacts
Chronic methaqualone use can have catastrophic long-term effects on both physical and mental health, emphasizing the importance of early intervention and treatment.
Health Consequences
- Liver damage
- Kidney dysfunction
- Neurological impairment
- Cardiovascular issues
Social and Economic Impact
Long-term users often encounter social isolation, financial hardships, and legal complications. These challenges can intensify the cycle of addiction, making recovery more arduous.
Broader Societal Effects
Methaqualone abuse not only harms individuals but also affects families, communities, and society as a whole. The drug's illegal trade fuels organized crime and undermines public health initiatives.
Economic Costs
The economic burden of methaqualone abuse includes healthcare expenditures, lost productivity, and law enforcement expenses. Addressing these issues necessitates a comprehensive strategy encompassing prevention, treatment, and enforcement.
Legal Framework and Regulation
Methaqualone is categorized as a Schedule I controlled substance in many countries, reflecting its high abuse potential and lack of accepted medical applications. Nonetheless, enforcement remains challenging in regions where illicit production and trafficking persist.
International Efforts
Global entities like the United Nations Office on Drugs and Crime (UNODC) collaborate to combat methaqualone trafficking through international cooperation and policy formulation. These initiatives aim to minimize the drug's availability and mitigate its impact on vulnerable populations.
Treatment Approaches for Methaqualone Abuse
Successful treatment for methaqualone addiction typically integrates medical and psychological interventions. Early intervention is critical for achieving favorable outcomes.
Detoxification
Medical detoxification aids in managing withdrawal symptoms and facilitates a secure transition to recovery. This process may incorporate medication-assisted treatment to alleviate discomfort and diminish cravings.
Counseling and Therapy
Behavioral therapies, such as cognitive-behavioral therapy (CBT), are instrumental in addressing the psychological dimensions of addiction. Support groups and aftercare programs offer continuous assistance throughout the recovery journey.
Prevention Strategies
Preventing methaqualone abuse requires a multi-faceted approach that includes education, community involvement, and policy development. By raising awareness and promoting healthier alternatives, individuals and communities can diminish the drug's allure.
Public Awareness Campaigns
Educational campaigns that highlight the dangers of methaqualone can dissuade potential users and encourage those affected to seek help. These efforts should focus on at-risk groups, including young people and marginalized communities.
Policy Recommendations
Strengthening enforcement mechanisms and enhancing access to treatment services are integral to an effective prevention strategy. Cooperation among governments, healthcare providers, and community organizations is crucial to achieving these objectives.
Conclusion
The repercussions of methaqualone on physical and mental health, alongside its societal impact, highlight the pressing need to address its misuse. By comprehending the drug's risks and advocating for prevention and treatment efforts, individuals and communities can collaborate to reduce its detrimental influence.
We urge readers to disseminate this article and engage in discussions about methaqualone and its effects. For those grappling with addiction, seeking professional help is the first step toward recovery. Together, we can foster a safer, healthier future for everyone.
Sources:
- World Health Organization (WHO)
- United Nations Office on Drugs and Crime (UNODC)
- National Institute on Drug Abuse (NIDA)